As anyone who works in healthcare will attest, patient-centered care has taken center stage in discussions of quality provision of healthcare, but has the true meaning of patient-centered become lost in the rhetoric? In this week’s Insights, we examine what it means to be truly patient-centered, using the eight principles of patient-centered care highlighted in research conducted by the Picker Institute and Harvard Medical School.
What is Patient-Centered Care?
Patient-centered care is the practice of caring for patients (and their families) in ways that are meaningful and valuable to the individual patient. It includes listening to, informing and involving patients in their care. The IOM (Institute of Medicine) defines patient-centered care as: “Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.”
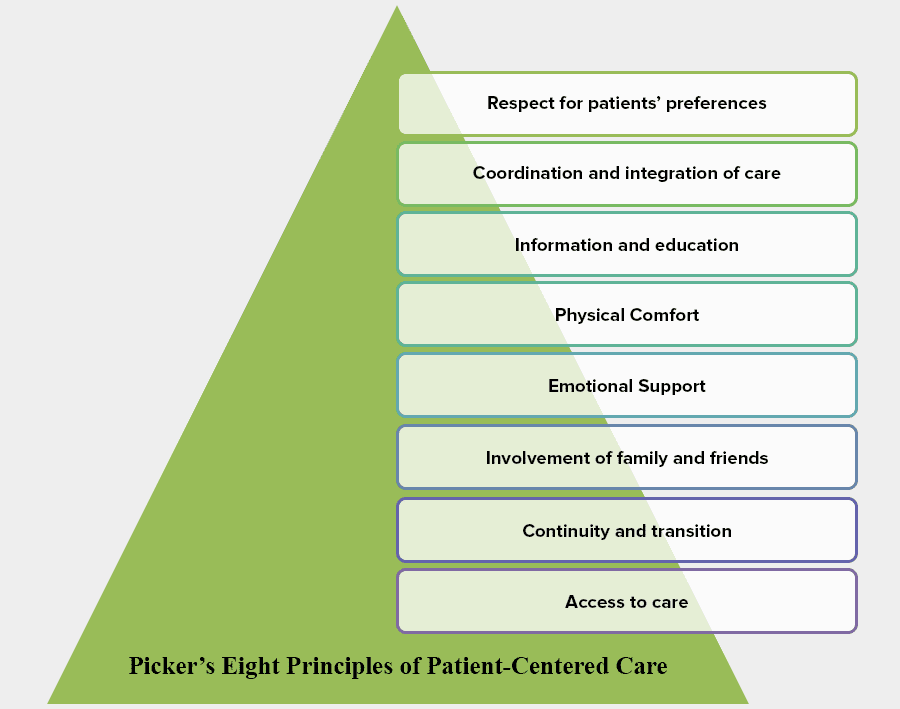
Overview of Picker’s Eight Principles of Patient Centered Care
Using a wide range of focus groups — recently discharged patients, family members, physicians and non-physician hospital staff—combined with a review of pertinent literature, researchers from Harvard Medical School, on behalf of Picker Institute and The Commonwealth Fund, defined seven primary dimensions of patient-centered care. These principles were later expanded to include an eighth – access to care. The researchers found that there are certain practices conducive to a positive patient experience and their findings form Picker’s Eight Principles of Patient-Centered Care.
1. Respect for patients’ values, preferences and expressed needs
Involve patients in decision-making, recognizing they are individuals with their own unique values and preferences. Treat patients with dignity, respect and sensitivity to his/her cultural values and autonomy.
2. Coordination and integration of care
During focus groups, patients expressed feeling vulnerable and powerless in the face of illness. Proper coordination of care can alleviate those feelings. Patients identified three areas in which care coordination can reduce feelings of vulnerability:
- Coordination of clinical care
- Coordination of ancillary and support services
- Coordination of front-line patient care
3. Information and education
In interviews, patients expressed their worries that they were not being completely informed about their condition or prognosis. To counter this fear, hospitals can focus on three kinds of communication:
- Information on clinical status, progress and prognosis
- Information on processes of care
- Information to facilitate autonomy, self-care and health promotion
4. Physical comfort
The level of physical comfort patients report has a significant impact on their experience. Three areas were reported as particularly important to patients:
- Pain management
- Assistance with activities and daily living needs
- Hospital surroundings and environment
5. Emotional support and alleviation of fear and anxiety
Fear and anxiety associated with illness can be as debilitating as the physical effects. Caregivers should pay particular attention to:
- Anxiety over physical status, treatment and prognosis
- Anxiety over the impact of the illness on themselves and family
- Anxiety over the financial impact of illness
6. Involvement of family and friends
This principle addresses the role of family and friends in the patient experience. Family dimensions of patient-centered care were identified as follows:
- Providing accommodations for family and friends
- Involving family and close friends in decision making
- Supporting family members as caregivers
- Recognizing the needs of family and friends
7. Continuity and transition
Patients expressed concern about their ability to care for themselves after discharge. Meeting patient needs in this area requires the following:
- Understandable, detailed information regarding medications, physical limitations, dietary needs, etc.
- Coordinate and plan ongoing treatment and services after discharge
- Provide information regarding access to clinical, social, physical and financial support on a continuing basis.
8. Access to care
Patients need to know they can access care when it is needed. Focusing mainly on ambulatory care, the following areas were of importance to the patient:
- Access to the location of hospitals, clinics and physician offices
- Availability of transportation
- Ease of scheduling appointments
- Availability of appointments when needed
- Accessibility to specialists or specialty services when a referral is made
- Clear instructions provided on when and how to get referrals.
At a global level, there is a seismic shift in thinking about empowering patients to take an active role in their care plan. At Oneview we see first-hand how technology can support patient-centred care, if used in the right way.
Institute of Medicine. “Crossing the Quality Chasm: A New Health System for the 21st Century”
What to learn more about our Care Experience Platform and how empathetic technology can power personalized, exemplary care experiences?



