When I became a nurse in 1998, I quickly learned that no matter the area of nursing, we were always “short-staffed” and the opportunity to pick up shifts was plentiful. It quickly became my habit to pick up shifts to help a unit or earn extra money for a household project or add to my savings account. Typically, by the start of the shift, our staffing needs were met and if they weren’t, the staffing office would work their magic or someone from the previous shift would graciously stay over, to ensure that we had enough staff to operate safely.
During the course of my career, there were certainly times when the “normal” short staffing was better or worse. There were times when events made nurses pause and think about their own risk before picking up extra shifts such as the H1N1 flu outbreak of 2009-’10 or the Ebola scare in 2014.
But historically nursing has always been a popular career path, so why do we have such a shortage now?
According to a study in October of 2021, nearly 1 in 5 Healthcare workers have quit their job in the United States. Since the beginning of COVID-19, 30% of healthcare workers have quit and 31% have considered leaving their employers – with 19% of those wanting to leave the field entirely.
So we enter The “Great Resignation Trifecta” – the three main areas that are currently forcing healthcare systems to change the way they are operating:
1. “Silver Tsunami”: There has been this looming “silver tsunami” that we’ve heard about for most of my career – the aging Baby Boomer population that was expected to severely strain health care providers, resources, and funding – compounded by the fact that many healthcare providers were also Baby Boomers and ultimately leading to an impending shortage of doctors and nurses. Well, the “Silver Tsunami” has arrived and an estimated 73 million people who are a part of this generation. The boomers are tech-savvy. They are well connected at home using internet, TV streaming, and 3rd party services like Netflix and they expect these same services when they are in the hospital. In order to increase or maintain their patient satisfaction scores, healthcare systems must revisit and re-prioritize technology projects.
2. Limited Nursing Resources: With more than 500,000 seasoned RNs anticipated to have retired by 2022 and the U.S. Bureau of Labor Statistics projecting the need for 1.1 million new RNs for expansion of the field and to replace the retirees, we can’t produce nurses fast enough! On top of that, we have a shortage of nursing professors to train our next generation of nurses. Coupled with nurse burnout and low job satisfaction, healthcare systems are looking for new and creative ways to increase staff satisfaction scores as well as to pump up their benefits packages. Two out of the three trifectas were anticipated, however, were not easily mitigated. Healthcare systems are looking for ways to automate manual workflows to increase efficiency and offload tasks from the bedside care staff. The current shortage is predicted to continue through 2030 so there is still time to make impactful adjustments.
3. COVID-19: The pandemic is nearing its third year and just as soon as things begin to calm down, a new variant pops up. After three years, the trifecta is taking a toll on healthcare workers. This is the reason so many health systems have been forced to innovate quickly and be as cost-effective as possible. We have seen “virtual” nursing programs rapidly implemented, hundreds of tablets swiftly deployed to support telemedicine in COVID-19 rooms, and many other smart ways to use technology to solve problems.
 As much as I hate to admit it, it seems that for the foreseeable future, this trifecta is here to stay.
As much as I hate to admit it, it seems that for the foreseeable future, this trifecta is here to stay.
As a vendor partner to our customers, we’ve heard first account stories of the strains the last few years have caused both on your margin and staffing. We’ve seen the public data regarding “the great resignation” and I’ve watched my friends and former colleagues switch employers and even leave their nursing careers as a result.
Now, more than ever, it is important to help lighten the load on the nursing staff and allow them to focus their time back to the bedside to take care of patients. Efficient and automated workflows lead to increased opportunities for nurses to provide care, leading to better patient outcomes, happier patients, happier nurses, and improved results.
By rapidly deploying a cloud based enterprise video solution, many of our customers were able to connect patients and families through video during very critical times and utilize telemedicine and virtual patient rounding to minimize staff exposure and risk as part of their COVID-19 response plan.
All the drivers of change for our customers are directly impacting the day-to-day operations at the hospital and indirectly affecting things such as profitability, staffing costs, patient outcomes (readmissions, adverse events), patient surveys, and staff satisfaction results.
A few prime examples:
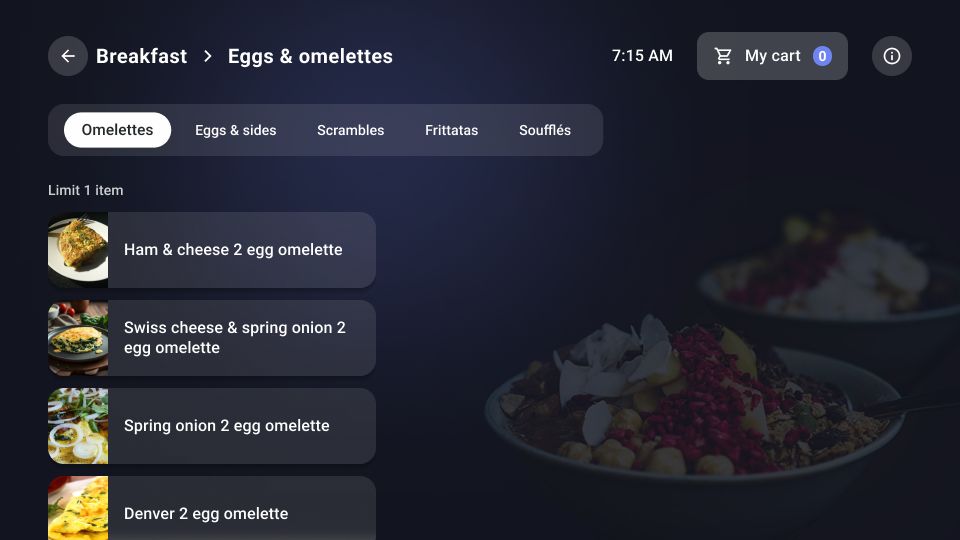
1. Meal Ordering: A well-integrated meal ordering user experience that allows the patient to automatically order trays, reducing the need to call orders to the dietary department. With over 749,600 meals ordered through Oneview since the start of the pandemic, we estimate that automatic meal ordering has saved over 10,400 hours in staff time.
2. Service Requests: Reducing call light volume by building service requests, which allow the patient to select and automatically request non-urgent, non-nursing needs using a notification framework. As excessive nurse call bells are avoided, this ultimately saves the on-duty nurse minutes of time.
3. Translation Services: Within a few clicks on the patient’s screen an on-demand translator, telemedicine visit, or zoom call can be placed 24/7 directly from the patient’s bedside device to connect to valuable resources
4. Telehealth Services: Using strategic positioning of the Oneview device and utilizing the Cisco Jabber app, staff can call into the room or monitor an isolation room via video. Supporting virtual interactions will help to reduce the need to enter an isolation room and save PPE (Personal Protective Equipment) costs.
These are just a few examples of how we have been able to come alongside our customers to support them as they are adapting to the ever-changing needs in healthcare.